Employee carjacked by two suspects at Kaiser Antioch Medical Center Tuesday
Wednesday, April 3rd, 2024
Adult male victim’s car recovered by police
By Allen D. Payton
An email from the “Kaiser Permanente Antioch Leadership Team” on Wednesday, April 3, 2024, alerted employees of a carjacking in one of the parking lots Tuesday afternoon. It was reported by an individual who chose to remain anonymous that the carjackers were armed and that “someone from administration said it was two high school kids and they caught them.” But that has not yet been confirmed by Antioch Police or Kaiser personnel.
UPDATE #1: However, according to Interim Police Chief Brian Addington, the suspects were not armed, as of 4:40 PM they have not been apprehended and APD will provide further information via a press release, later.
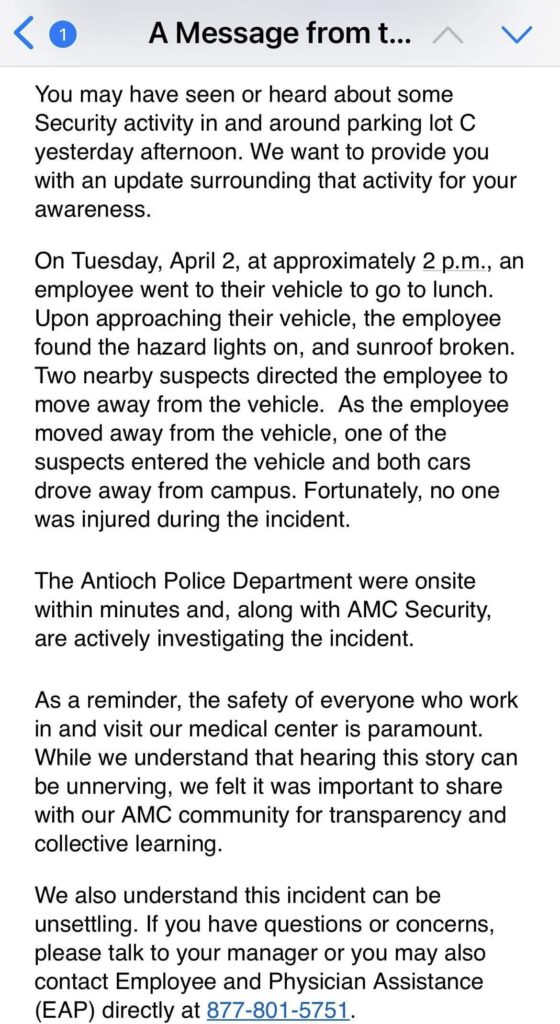
The email reads, “You may have seen or heard about some Security activity in and around parking lot C yesterday afternoon. We want to provide you with an update surrounding that activity for your awareness.
On Tuesday, April 2, at approximately 2 p.m., an employee went to their vehicle to go to lunch. Upon approaching their vehicle, the employee found the hazard lights on, and sunroof broken. Two nearby suspects directed the employee to move away from the vehicle. As the employee moved away from the vehicle, one of the suspects entered the vehicle and both cars drove away from campus. Fortunately, no one was injured during the incident.
The Antioch Police Department were onsite within minutes and, along with AMC Security, are actively investigating the incident.
As a reminder, the safety of everyone who work in and visit our medical center is paramount. While we understand that hearing this story can be unnerving, we felt it important to share with our AMC community for transparency and collective learning.
We also understand this incident can be unsettling. If you have any questions or concerns, please talk to your manager or you may also contact Employee and Physician Assistance (EAP) directly at 877-801-5751.”
UPDATE #2: According to an Antioch Police press release issued at 5:58 PM by Acting Captain Desmond Bittner of the Community Policing Bureau, “On April 2, 2024, at approximately 1:13 PM, Antioch Police Officers responded to 4501 Sand Creek Road (Kaiser Antioch) for a reported carjacking that had just occurred. When officers arrived, they learned the victim, (an adult male), had interrupted several suspects in the process of stealing his vehicle. One suspect confronted the victim, causing the victim to fear for his safety.
The suspects left in the victim’s vehicle towards Sand Creek Road. Antioch Police Officers later recovered the victim’s vehicle in a nearby neighborhood, unoccupied. Through the initial investigation several investigative leads were obtained. The investigation was forwarded to the Antioch Police Department’s Investigations Bureau.
This preliminary information is made available by the Community Policing Bureau. Any further information or additional inquiries can be directed to Detective Cole Shaffer at 925-779-6944 or by emailing cshaffer@antiochca.gov.”