Learn about Dementia Caregiving During the Holidays from TreVista Antioch Tuesday, Nov. 26
Monday, November 25th, 2024


Earns an “A” for limiting patient injuries, reducing medical errors, and preventing infections, according to The Leapfrog Group
By Antonia Ehlers, PR and Media Relations, Kaiser Permanente Northern California
Antioch, CA – Kaiser Permanente Antioch is being recognized as among the safest in the nation for patient care, according to The Leapfrog Group’s biannual Hospital Safety Grades report.
Leapfrog reviews hospital clinical data and assigns hospitals grades based on approximately two dozen safety measures that analyze patient injuries, medical and medication errors, and infections. Kaiser Permanente Antioch is recognized with an “A” grade for patient safety.
“We putpatient safety at the forefront of everything we do,” said Kaiser Permanente Diablo Senior Vice President and Area Manager Pam Galley. “This recognition highlights the safe, high-quality care our physicians, nurses and staff provide every day to our members and patients.”
This fall, 14 Kaiser Permanente hospitals in Northern California received A grades from Leapfrog, including: Antioch, Fresno, Manteca, Modesto, Oakland, Roseville, San Francisco, San Jose, San Leandro, San Rafael, Santa Clara, Santa Rosa, South Sacramento, and South San Francisco.
“Being among the top hospitals in the nation for patient safety is part of Kaiser Permanente’s commitment to provide safe care that improves the overall health and well-being of our members and patients,” said Kaiser Permanente Antioch Physician in Chief Sharon Mowat, MD. “Our dedicated clinical teams are focused on keeping our patients and members safe in a warm and welcoming environment.”

The Leapfrog Group assigns letter grades to nearly 3,000 hospitals throughout the United States. The grades are updated twice annually, in the fall and spring.
More than 60% of Kaiser Permanente Northern California hospitals received an A grade. In California overall, only about 30% of the state’s hospitals earned this top grade.
The Leapfrog Group, an independent national nonprofit run by employers and other large purchasers of health benefits, released its Hospital Safety Gradesafter examining publicly available data on patient injuries, medical and medication errors, and infections at U.S. hospitals. The report includes data collected by national health care organizations, including the Centers for Disease Control and Prevention and the U.S. Department of Health and Human Services. Scores are calculated based on more than two dozen publicly available measures, and hospitals are then assigned A, B, C, D or F grades for their safety records. The grades are released as a free resource to help patients and their families make informed health care decisions.
Kaiser Permanente is one of America’s leading integrated health care providers and serves 12.5 million members. Nationally, 24 of the 39 Kaiser Permanente hospitals that were eligible for a grade, more than 60% percent, received a Leapfrog Safety A grade. In contrast, approximately 30% of the nation’s hospitals received an A rating.
For complete details on Kaiser Antioch’s grade click, here and for more information and a complete list of the hospital safety grades, visit Leapfrog.
By Christeen Tilenius

According to “Mental Health America” in 2024, one in four adults with mental distress couldn’t get help because they couldn’t afford it. In hopes of helping people in Antioch to be able to afford help with their mental health if they want it, I am sharing this information with you.
I sadly had a friend who could not afford to get the help they needed with their anxiety and self-medicated themselves with alcohol to numb it. They died young after being run over by a car while walking in the middle of a busy road at night while drunk. I always wondered if they wouldn’t have turned to alcohol, and died young if they had been able to get the help they needed with their anxiety.
We often write-off our anxiety as stress and call it “normal”, as if there is no way to escape our discomfort due to the day and age we live in. There is a difference between stress and anxiety just as there is a difference between getting sad and having depression. Most importantly, we can help ourselves to start to feel better regardless of what we call our emotional discomfort.
It is obvious that we are injured when we have a broken leg and can just barely limp along with a cast on crutches. It is easy for all people to see when someone has a broken leg, but sometimes only we know if we are hurting emotionally. When we have a broken dream, promise, relationship or heart, regrets that won’t leave us alone or failures that continue to haunt us, we can feel just as hurt or worse than if we had a broken leg.
An analysis appearing in 2011 in the journal Psychiatric Times reports that up until that year over 20 studies had examined brain changes after therapy for depression, anxiety disorders, obsessive-compulsive and related disorders, and trauma disorders like PTSD; all found that therapy changes the brain as much as psychiatric medication. Please note that I am not in any way telling people who need medication to not take it.
There are local mental health therapists, who take various types of health insurance, provide free services and sliding scale services to help people to cope regardless of their income levels. If time is a stressor, you may be able to find a therapist who can help you with regular phone calls or telehealth meetings. California State Licensed therapists go through 8+ years of college education in order to practice in the state of California, often a testament to their desire to help you feel better. In closing, please remember that all people experience challenges at points in their lives and there is no shame in asking for help.
Here is the contact information for some of the free, low-cost, sliding scale therapy services and crisis hotlines available to Antioch, California residents:
1) Mental Health Services for Adults & Caregivers
www.cchealth.org/get-care/mental-health
Contra Costa Health Services (CCHS) – Behavioral Health Services (BHS)
Call the 24/7 ACCESS Line at 1-888-678-7277
2) Brighter Beginnings Family Health Clinic Antioch Behavioral Therapy
3505 Lone Tree Way, Antioch, CA 94509, (925) 303-4780
3) Lifelong East Oakland Health Center
10700 MacArthur Blvd., Oakland, CA 94605, (510) 981-4100
4) Mobile Therapy by God’s Love Outreach Ministries (GLOM)
www.godsloveoutreach.com, (925) 999-4119
5) YWCA Contra Costa/Sacramento
1320 Arnold Drive, Suite 170, Martinez, CA 94553, 925-372-4213 ext. 123
6) Community Clinic Psychotherapy Services
2232 Carleton Street Berkeley, California, 94704, (510) 548-2250
7) Center for Psychotherapy
509 W 10th Street, Antioch, CA 94509, (925) 777-9540
8) Community Health for Asian Americans
3727 Sunset Lane, Antioch, CA 94509, (925) 778-1667
9) The Crisis Center’s Crisis Lines
Provide crisis and suicide intervention, emotional support, counseling and resource information for Contra Costa County. This program provides 24/7 Support via Call or Text. If you are in a crisis and need help immediately, please call 211 or 800-833-2900 or text ‘‘HOPE” to 20121 now. Doing so will quickly put you in touch with one of the program’s call specialists.
10) National Domestic Violence Hotline
1 (800) 799-7233 or text START to 88788
NOTE: In an emergency dial 911

High rating reflects the expert medicine, seamless care and outstanding service provided to Kaiser’s 1.4 million Medicare Advantage members
By Antonia Ehlers, PR and Media Relations, Kaiser Permanente Northern California
OAKLAND, CA — Kaiser Permanente’s Medicare health plan in California is rated among the best in the state for providing high-quality, seamless care, and outstanding service to its 1.4 million Medicare Advantage members.
This year, the Kaiser Permanente Medicare health plan in California received 4.5 out of 5 stars, according to the Centers for Medicare & Medicaid Services (CMS) 2025 Star Ratings. In addition, the Kaiser Permanente Medicare health plan in California is tied for the highest star rating in the state.

“These ratings demonstrate our commitment to providing high-quality care and exceptional service to all of our Northern California members, including our Medicare Advantage members,” said Carrie Owen Plietz, FACHE, president of Kaiser Permanente’s Northern California region. “Kaiser Permanente is routinely recognized as being among the nation’s best for improving the health and well-being of our members and patients.”
The Kaiser Permanente Medicare health plan in California has been highly rated – with mostly 4.5 and 5 star ratings – for the past 15 years.
“Our clinicians work together across all specialties to ensure personalized, high-quality care for our patients,” said Maria Ansari, MD, FACC, CEO and executive director of The Permanente Medical Group. “The CMS Star Ratings, along with our nation-leading NCQA ratings, demonstrate the commitment of our physicians and care teams to provide all of our patients with the exceptional and compassionate care they need to live long, healthy lives.”
Ratings reflect high-quality care and service
Every year, CMS publishes Medicare Advantage (Part C) and Medicare prescription drug plan (Part D) ratings. The ratings offer consumers a way to compare the quality of Medicare plans.
To develop the ratings, CMS considers many areas of care and service. For example, it looks at how well health plans keep members healthy and manage their chronic conditions. CMS also considers patient experiences, customer service, patient access, and pharmacy services.
Kaiser Permanente provides care to more than 1.9 million Medicare members in 8 states and the District of Columbia.
Northern and Southern California are rated together as one contract with CMS. Kaiser Permanente’s Dual Eligible-Special Needs Plan (D-SNP) H-contract (H8794) began in California on January 1, 2024, and is too new to be measured for the 2025 Star Ratings. It will be eligible beginning with the 2026 Star Ratings if the contract has sufficient enrollees and measures rated.
Ongoing recognition for Kaiser Permanente’s health plans
The National Committee for Quality Assurance (NCQA) also recently ranked Kaiser Permanente Northern California’s health plans as the highest rated in California – and among the highest in the nation – for providing expert, coordinated care, and exceptional service.
Kaiser Permanente’s Medicare and commercial health plans in Northern California each received 4.5 out of 5 stars, according to NCQA’s 2024 Health Plan Ratings. This was the ninth ratings period that Kaiser Permanente Northern California was the highest-rated plan in the region and among the highest in the country. Nationally, only 8% of the health plans are rated 4.5 stars or higher.
NCQA also ranked Kaiser Permanente Northern California health plans as best in the state for overall treatment, prevention, equity, and patient experience.
Enrolling in a Kaiser Permanente Medicare Health Plan
Medicare’s annual enrollment period for all 2025 Medicare health plans begins on October 15 and runs through December 7, 2024.
Medicare beneficiaries can learn more about the CMS’ star ratings and Kaiser Permanente’s Medicare health plans by visiting kp.org/medicarestars.
About Kaiser Permanente
Kaiser Permanente is committed to helping shape the future of health care. We are recognized as one of America’s leading health care providers and not-for-profit health plans. Founded in 1945, Kaiser Permanente has a mission to provide high-quality, affordable health care services and to improve the health of our members and the communities we serve. We currently serve more than 12.5 million members in 8 states and the District of Columbia. Care for members and patients is focused on their total health and guided by their personal Permanente Medical Group physicians, specialists, and team of caregivers. Our expert and caring medical teams are empowered and supported by industry-leading technology advances and tools for health promotion, disease prevention, state-of-the-art care delivery, and world-class chronic disease management. Kaiser Permanente is dedicated to care innovations, clinical research, health education, and the support of community health. For more information, go to about.kp.org.

Application period for Kaiser Permanente’s Community Health Care Program opens Nov. 1st
By Antonia Ehlers, PR and Media Relations, Kaiser Permanente Northern California
Many low-income Californians make too much money to qualify for Medi-Cal, but they’re unable to get affordable health coverage anywhere else. Kaiser Permanente’s Community Health Care Program (CHCP) was designed with them in mind.
The Kaiser Permanente CHCP provides comprehensive, affordable health care coverage for qualified low-income adults and children in California who don’t have access to other public or private health coverage.
Open enrollment for CHCP is Nov. 1, 2024, through Jan. 31, 2025.
Eligible Californians receive comprehensive health coverage from Kaiser Permanente including preventive services, without paying a monthly premium. They also don’t pay copays or out-of-pocket costs for most care at Kaiser Permanente facilities.
“Even with the expansion of Medi-Cal in 2024, too many Californians remain uninsured,” said Yvette Radford, vice president, External and Community Affairs, Kaiser Permanente Northern California. “The Community Health Care Program helps address this gap, providing Kaiser Permanente’s high-quality care and coverage to eligible Californians in our service areas.”
Who is eligible for the Community Health Care Program?
The program is designed for applicants who meet the following criteria:
• total household annual income of no more than 3 times the federal poverty level (Example: up to $45,180 for an individual or up to $93,600 for a family of 4 in 2024)
• not eligible for any other health coverage, including Medi-Cal, Medicare, a job-based health plan, or Covered California
• must live in a Kaiser Permanente California service area
Individuals do not have to be U.S. citizens to qualify. Applications must be submitted by January 31, 2025.
How to apply
As of November 1, you can apply online at www.kp.org/chcp. Click the “apply now” button at the top of the website for a link to the application. If you need assistance, click the “get help” button for a list of community agencies that can provide help, or call Kaiser Permanente Member Services at 1-800-464-4000 (TTY 711).
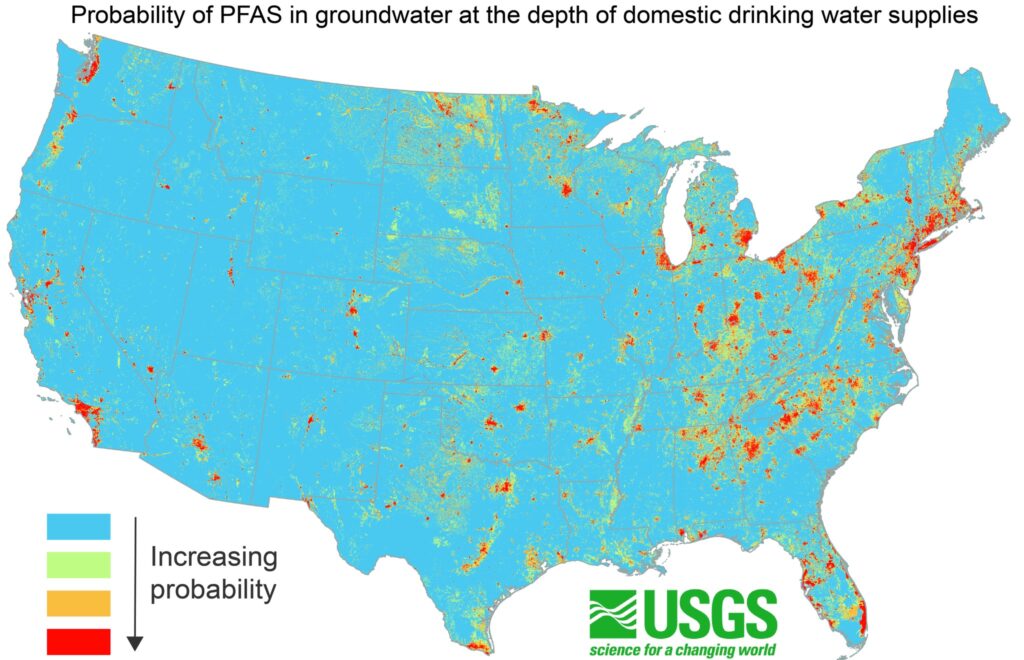
Estimates according to a new USGS predictive model. Exposure to some PFAS may lead to adverse health risks.
Antioch has some of the highest levels
Approximately 71 to 95 million people in the Lower 48 states – more than 20% of the country’s population – may rely on groundwater that contains detectable concentrations of per- and polyfluoroalkyl substances, also known as PFAS, for their drinking water supplies. These findings are according to a U.S Geological Survey study published Oct. 24. The predictive model results can help members of the public, water suppliers and regulators understand the potential for PFAS contamination, guide future studies and inform strategic planning for water resources.
USGS scientists are the first to report national estimates of PFAS occurrence in untreated groundwater that supplies water to public and private wells. This research also provides the first estimate of the number of people across the country who are potentially affected by PFAS-contaminated groundwater.
Along with a scientific report, the USGS published an interactive, online map so users can see probability estimates of PFAS occurrence. Note that predictive results are intended to be evaluated at state, regional and national scales rather than at individual household levels. Probability estimates are for the presence of PFAS in groundwater and do not account for any subsequent actions taken by states, municipalities or individuals to treat drinking water. The model does not include estimates of PFAS concentrations; testing is the only way to confirm the presence of contaminants.

Exposure to certain PFAS may lead to adverse health risks in people, according to the U.S. Environmental Protection Agency. PFAS are a group of synthetic chemicals used in a wide variety of common applications, from the linings of fast-food boxes and non-stick cookware to fire-fighting foams and other purposes. PFAS are commonly called “forever chemicals” because many of them do not easily break down and can build up over time, making them a concern for drinking water quality.
“This study’s findings indicate widespread PFAS contamination in groundwater that is used for public and private drinking water supplies in the U.S.,” said Andrea Tokranov, USGS research hydrologist and lead author of this study. “This new predictive model can help prioritize areas for future sampling to help ensure people aren’t unknowingly drinking contaminated water. This is especially important for private well users, who may not have information on water quality in their region and may not have the same access to testing and treatment that public water suppliers do.”
The EPA has established legally enforceable levels, called maximum contaminant levels, for six types of PFAS in drinking water. The EPA regulates public water supplies, and some states have additional regulations for drinking water. Some homes use private water supplies, where residents are responsible for the maintenance, testing and treatment of their drinking water. Those interested in treatment processes and testing options can read EPA’s guidance or contact their state officials or water supplier.
The states with the largest populations relying on public water supplies with potentially contaminated groundwater sources are Florida and California. Regarding private wells, Michigan, Florida, North Carolina, Pennsylvania, New York and Ohio have the largest populations relying on potentially contaminated groundwater.
The study also presents data according to population percentage. In Massachusetts, for example, the source water for 86 to 98% of people who rely on groundwater from public water supplies could be contaminated with PFAS. In Connecticut, the source water for 67 to 87% of the people who rely on groundwater from private wells could be affected. Details by state can be seen in the report’s tables S6 through S8.
“To derive these estimates, the team analyzed 1,238 groundwater samples collected by USGS scientists and determined how factors such as urban development and well depth can impact PFAS occurrence,” continued Tokranov. “With that information, a detailed machine learning model was developed and used to identify which geographic areas have a higher likelihood for contamination. That information was combined with existing USGS research on the number of people in a given area who rely on groundwater for drinking water to establish population estimates.”
Scientists present separate estimates for public and private wells because they typically receive water from different groundwater depths. Public wells using groundwater as the primary water source are usually deeper than private wells.
There are more than 12,000 types of PFAS, not all of which can be detected with current tests; the USGS study tested for the presence of 24 common types. The USGS estimates consider the presence of at least one of those 24 types of PFAS. The most frequently detected compounds were perfluorobutane sulfonate known as PFBS, perfluorooctane sulfonate known as PFOS and perfluorooctanoate known as PFOA.
This research provides a broad outlook for the Lower 48 states and presents state-level estimates. Scientists did not look in detail at specific cities or provide estimates for the types of PFAS present or PFAS concentrations.
The new USGS study was published in Science.
Learn more about USGS research on PFAS by reading the USGS strategy for the study of PFAS in the environment and visiting the USGS PFAS Integrated Science Team’s website.
For more information about PFAS regulations, visit the EPA’s website on addressing PFAS.

By Antioch Police Department
Join us this Saturday, October 26th, from 10 am to 2 pm at the DEA Take Back event! Dispose of your unused medications safely and anonymously at convenient local drop-off locations nationwide. Locate a collection site near you: www.DEATakeBack.com.
Solid and liquid medications may be disposed. No medical sharps will be accepted.
Where: Antioch Police Department
300 L Street, Antioch
Inside the front lobby
From 10:00am to 2:00 pm.

By Nola Woods, Public Affairs Director, Contra Costa Mosquito and Vector Control District

The Contra Costa Mosquito and Vector Control District (District) confirms more of the invasive mosquito species Aedes aegypti have been found earlier this month at various locations in Antioch. This mosquito species, which has the common name, the Yellow Fever mosquito, is capable of transmitting Zika, dengue fever, Chikungunya, and yellow fever viruses. In response, the District will continue to perform more door-to-door inspections on Saturdays in the area bordered by Highway 4 to the north, Bluerock Drive to the south, Lone Tree Way to the west, and Deer Valley Road to the east.
The District first identified Aedes aegypti mosquitoes in Antioch in late September, when they were collected during a backyard inspection. As additional trapping and inspections were conducted in the neighborhood, more invasive mosquitoes were found prompting the District to set mosquito traps throughout the area and conduct door-to-door inspections to determine how widespread the infestation is. During these inspections, we have found mosquito larvae (young mosquitoes) in common backyard items that can hold water, including potted plant saucers, buckets, wheelbarrows, fountains, and toys. As more adult and young mosquitoes are found, the District’s search area continues to expand.

“The fact that we continue to find young and adult mosquitoes as we expand our search area suggests this mosquito population may have been in Antioch for at least several months. We will continue to conduct surveillance and inspections until the weather cools this year and mosquito activity becomes less likely,” said Steve Schutz, Ph.D., Scientific Programs Manager.
Aedes aegypti mosquitoes are very small (about 1/4 inch), with black bodies and white stripes. They were first introduced to Southern California more than 10 years ago. Since then, they have moved from Southern California to Shasta County and are now established in 24 counties across the state. Because these mosquitoes lay sticky eggs above the water line in any size container that holds water, they can be transported to new areas easily and are often introduced through travel, particularly as people move from area to area and accidentally transport these mosquitoes in potted plants or other outdoor containers.
To reduce the risk of these mosquitoes, it is important that residents:
Contra Costa Mosquito and Vector Control District, an independent special district and public health agency, is located at 155 Mason Circle in Concord.